Experts Urge Caution as Trump’s “Big” Bill Pushes AI Adoption in Rural Healthcare
Washington, D.C. — The Trump administration has unveiled the parameters of its new “Rural Health Transformation Fund,” a key component of the president’s “big, beautiful” healthcare bill. The initiative offers $50 billion in funding over a five-year period to states that agree to modernize their medical infrastructure. However, to qualify for these federal dollars, states are required to satisfy at least three out of ten distinct criteria. Among the most prominent of these requirements is the mandatory integration of artificial intelligence (AI) and other advanced technologies into healthcare settings.
While the funding aims to bolster rural healthcare networks, experts are raising alarms regarding the financial reality behind the bill. Analysts point out that the $50 billion designated for the Rural Health Transformation Fund is significantly overshadowed by broader cuts contained within the legislation. The Congressional Budget Office (CBO) projects a reduction in Medicaid spending totaling $911 billion over the coming decade. These substantial cuts are expected to impact both low-income patients who rely on Medicaid for free health coverage and the hospitals that depend on Medicaid reimbursements to remain operational.

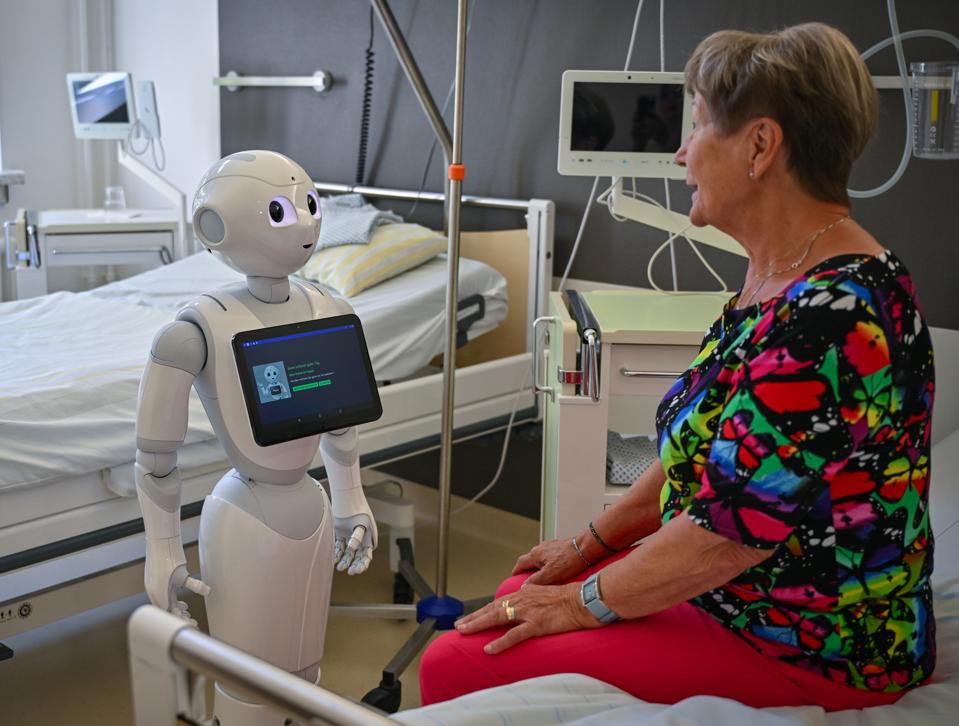
Despite the fiscal concerns, experts in the field of technology and medicine see potential benefits in the bill’s technological push. The legislation specifically calls for “consumer-facing, technology-driven solutions for the prevention and management of chronic diseases.” Furthermore, it mandates training and technical assistance for adopting solutions such as remote monitoring, robotics, and artificial intelligence to improve care delivery in rural environments.
Chenhao Tan, an associate professor of data science at the University of Chicago, and Karni Chagal-Feferkorn, an assistant professor at the University of South Florida’s college of AI and cybersecurity, suggest that AI could serve as a vital lifeline for rural hospitals. These facilities are frequently defined by their lack of resources and chronic under-staffing. Both professors agree that AI technology has the capacity to significantly reduce the crushing administrative burden that physicians at these hospitals face daily.
According to data from the American Medical Association, physicians are responsible for taking detailed notes on patient visits and compiling them for electronic health records systems—a task that can consume eight hours or more of their work week. This administrative load often contributes to physician burnout, a critical issue in the medical community.
A recent study highlighted by the experts found that while patient notes generated by AI are generally worse than those created by expert physicians, they are similar in quality to those produced by general physicians. Professor Tan emphasized the importance of context when evaluating these risks and benefits, particularly in stressed rural environments.
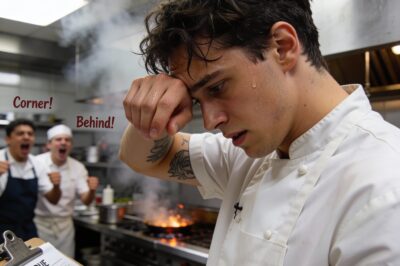
“If the baseline is tired human doctors, then I think it is even easier to make an argument that AI may do better than them,” Tan stated, noting that the comparison must account for the fatigue and workload human doctors endure.
Professor Chagal-Feferkorn expressed hope that the integration of AI could help alleviate staffing shortages in rural areas, not just by reducing workloads but by making these positions more attractive to medical professionals.
“If the equipment is state-of-the-art, and they feel that much of the burdensome work is done by AI, I think this could be one incentive for physicians to go work in rural areas, this might have a great impact,” Chagal-Feferkorn said.
However, the regulatory landscape for these technologies remains a point of concern. The Food and Drug Administration (FDA) currently regulates AI technologies intended to evaluate and diagnose health conditions, classifying them as medical devices. In contrast, technologies that simply transcribe and compile patient notes fall outside this regulatory framework, even though they often market themselves as being compliant with HIPAA privacy standards.
Tan remarked that expecting these new technologies to be “bulletproof” before entering the market might be an unrealistically high bar, but he insisted that “there should be something higher than nothing” regarding regulatory requirements.
Beyond regulation, the proliferation of AI in healthcare networks introduces new cybersecurity vulnerabilities. Chagal-Feferkorn warned that “AI makes it easier for ordinary people to hack systems.” While she acknowledged that AI could improve patient safety by merging records from different providers—ensuring, for example, that every provider is aware of a patient’s full medication list to avoid dangerous interactions—this interconnectedness comes with trade-offs.
“The more data sharing there is, obviously the risk for data security breach is larger,” Chagal-Feferkorn continued.
To mitigate these risks, Tan argued that “worker upscaling needs to go hand in hand” with the adoption of any new AI technology. Both Tan and Chagal-Feferkorn expressed a shared concern that under-resourced hospitals, driven by the financial pressures of the new bill, might attempt to adopt AI technology primarily as a cost-cutting measure without investing in the necessary staff training and safety infrastructure required to operate it safely.
News
Taylor Swift and Travis Kelce Invest $11 Million in ‘Music and Justice’ to Spotlight Virginia Giuffre’s Story
Taylor Swift and Travis Kelce Launch ‘Music and Justice’: An $11 Million Initiative to Confront Historical Silence In a move…
President Trump Addresses Newly Released Photos Linked to Jeffrey Epstein Inquiry
President Trump Brushes Off New Epstein Photos Amid House Oversight Committee Release WASHINGTON, D.C. — President Donald Trump has publicly…
Gifted Hands: He Was Born in Poverty, Raised in Anger, and Destined to Separate the Inseparable
Part 1 I was the kid everyone made fun of. Growing up in Detroit, I wasn’t just poor; I was…
The $300,000 Miracle Inside a Tomato Can: How a Secret Inheritance Saved My Family from Being Evicted in Chicago
Part 1: The Return to the Grinder It’s 6:00 AM in Chicago. The wind coming off the lake cuts right…
ALONE IN ALASKA: I Thought I Could Handle the Storm, But Nature Had Other Plans
Part 1 The cold isn’t just a temperature up here in Alaska; it’s a predator. And right now, it’s hunting…
Facing 20 Years In A Leavenworth Prison Cell For Saving Lives: The Untield Story Of The “Ghost” Pilot Who Turned Off His Radio To Save An Ambushed Unit
Part 1 The cockpit of an A-10 Thunderbolt is usually the loudest place on earth, a titanium bathtub strapped to…
End of content
No more pages to load